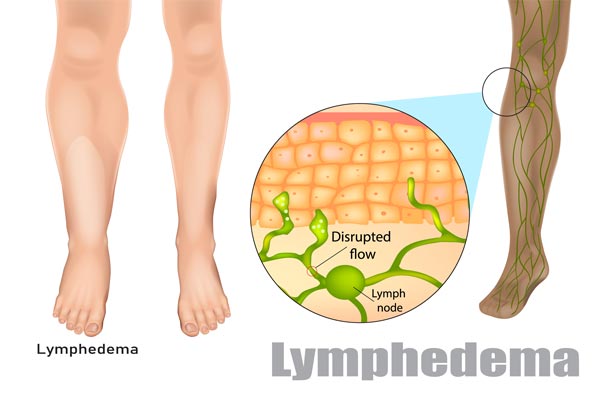
What Causes LymphedemaLymphedema impacts millions of people in the United States and occurs when the body cannot effectively transport lymph fluid. When transport is disrupted and lymph fluid cannot drain properly, swelling occurs. This swelling can be in any part of the body, most often in the arms and legs, but also the breast or chest wall, head and neck, or genitals.
While there is no absolute cure for lymphedema, significant progress has been made in the management of the disease, including the ability to detect early onset lymphedema so that living with chronic debilitating lymphedema can become a thing of the past! A DISEASE THAT IMPACTS MILLIONS, BUT IS ONLY KNOWN BY A FEW |
Lymphedema occurs when there is abnormal accumulation of protein-rich fluid, which usually causes chronic inflammation and reactive fibrosis. The lymphatic system can be thought of as the “garbage disposal” system of the body. The job of the lymphatic system is to pick up the excess fluid, which leaks out at the capillary level, take it to the lymph nodes where it is filtered and concentrated, and then dump it back into the cardiovascular system. The lymph nodes also serve as an important immune role to help prevent spread of infection and cancer.
PRIMARY AND SECONDARY LYMPHEDEMA
There are two types of lymphedema – primary and secondary. Both types relate to lymph vessels or lymph nodes that are missing, damaged, removed or otherwise impaired. Additionally, lymphedema can be classified as benign or malignant.
Primary Lymphedema
Primary lymphedema is due to a developmental defect (malformation, dysplasia) of the lymph vessels and/or lymph nodes. Primary lymphedema can be either congenital or hereditary.
Secondary Lymphedema
Secondary lymphedema is caused by an insult to the lymphatic system and can appear at any age. Causes may include:
- Surgery/radiation for cancer: Lymph node dissection that is often associated with cancer therapy can disrupt lymph flow.
- Radiation for cancer: Radiation can cause tissue fibrosis which can impair lymph flow.
- Cancer. Malignant tumors can grow and compress lymph vessels and decrease flow. Also, cancer cells can penetrate lymph vessels and multiply and block flow.
- Trauma: Crushing injuries, burns, and other traumas to the body can affect the lymphatic vessels inhibiting flow.
- Infection: Chronic or recurrent bouts of acute lymphangitis (infection of the lymph vessels) can cause damage to the lymphatic vessels.
- Chronic Venous insufficiency: Improper functioning of the vein valves in the legs can create constant increased strain on the lymphatic system and ultimately cause lymphatic insufficiency.
- Obesity: The increased lymphatic load associated with obesity, often in conjunction with increased pressure on lymph nodes, can impair lymphatic flow.
Progression of Lymphedema
Progression of lymphedema to irreversible stages is due to the body’s inflammatory response over time as it tries to get rid of the proteins in the interstitial fluid. The inflammatory response leads to tissue fibrosis (thickening or scarring) and deposition of fatty tissue. Some people develop fibrosis and fatty tissue deposition very quickly, and some go years and have very little irreversible changes. We do not understand all the factors. Some factors are likely genetic, but diet and healthy living may play a role in reducing the inflammatory response as well. Inflammation is also thought to lead to further damage to the remaining lymphatic vessels over time, as they are very fragile.
When transport is stopped and lymph fluid cannot drain properly, it causes swelling distal to the area where the drainage is disrupted. This swelling can be in any part of the body, most often in the arms and legs, but also the breast or chest wall, head and neck, or genitals.
When transport is stopped and lymph fluid cannot drain properly, it causes swelling distal to the area where the drainage is disrupted. This swelling can be in any part of the body, most often in the arms and legs, but also the breast or chest wall, head and neck, or genitals.